Covid in Norway: 'significant' excess all-cause mortality in 2021-22, with 'cardiovascular diseases' going through the roof
Raknes et al. bring 'new' data from Norway, which points to 'something' that happened from Q2 2021 onwards (but it remains, of course, outside the paper)
And now I’ll bring you…the study ‘Excess non-COVID-19 mortality in Norway 2020–2022’ by Raknes et al., BMC Public Health (2024) 24:244.
Emphases and bottom lines mine; for readability, I’ve omitted the references (please consult the fully open access version linked above for them)..
Abstract
Background Causes of death other than COVID-19 seem to contribute significantly to the excess mortality observed during the 2020–2022 pandemic. In this study, we explore changes in non-COVID-19 causes of death in Norway during the COVID-19 pandemic from March 2020 to December 2022.
Methods We performed a population-based cross-sectional study on data from the Norwegian Cause of Death Registry. All recorded deaths from 1st January 2010 to 31st December 2022 were included. The main outcome measures were the number of deaths and age-standardised death rate (ASMR) per 100000 population from the major cause of death groups in 2020, 2021 and 2022. The predicted number of deaths and ASMRs were forecasted with a 95% prediction interval constructed from a general linear regression model based on the corresponding number of deaths and rates from the preceding ten prepandemic years (2010–2019). We also examined whether there were deviations from expected seasonality in the pandemic period based on prepandemic monthly data from 2010–2019. The cumulative number of deaths and ASMR were estimated based on monthly mortality data.
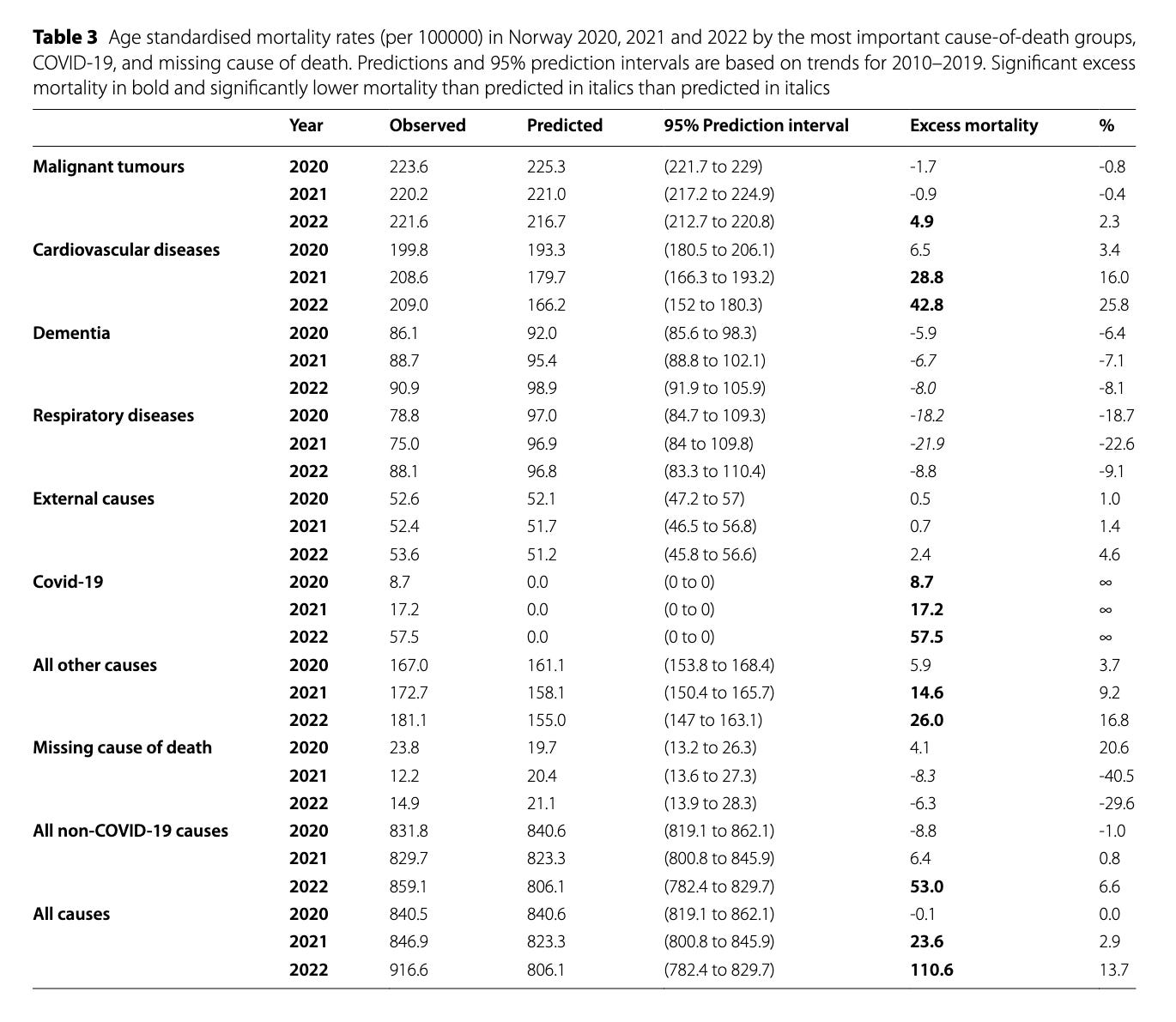
Results There was significant excess mortality (number of deaths) in 2021 and 2022 for all causes (3.7% and 14.5%), for cardiovascular diseases (14.3% and 22.0%), and for malignant tumours in 2022 (3.5%). In terms of ASMR, there was excess mortality in 2021 and 2022 for all causes (2.9% and 13.7%), and for cardiovascular diseases (16.0% and 25,8%). ASMR was higher than predicted in 2022 for malignant tumours (2.3%). There were fewer deaths than predicted from respiratory diseases (except COVID-19) in 2020 and 2021, and from dementia in 2021 and 2022. From March 2020 to December 2022, there were cumulatively 3754 (ASMR 83.8) more non-COVID-19 deaths than predicted, of which 3453 (ASMR: 79.6) were excess deaths from cardiovascular disease, 509 (ASMR 4.0) from malignant tumours. Mortality was lower than predicted for respiratory diseases (-1889 (ASMR: -44.3)), and dementia (-530 (ASMR-18.5)).
Conclusions There was considerable excess non-COVID-19 mortality in Norway from March 2020 until December 2022, mainly due to excess cardiovascular deaths. For respiratory diseases and dementia, mortality was lower than predicted.
What’s in a Percentage?
What a—bummer. Did you catch the main points? ‘Significant excess mortality’, esp. due to cardiovascular diseases and malignant tumours (cancers), with esp. the former driving these developments.
This is what a ‘signal’ looks like:
Statistical methods
Handling of data and statistical analyses were carried out in Toad for Oracle and Microsoft Excel. The number of deaths and ASMRs for 2020, 2021, and 2022 were compared with data from 2010 to 2019. Age-standardised mortality rates were computed by the direct standardisation method, using 5-year age strata and the European Standard Population of 2013 as the standard population. The ‘at risk’ population was defined as the Norwegian mean population according to Statistics Norway for each year.
The observed number of deaths and death rates of 2020, 2021 and 2022 were compared with projections based on yearly data 2010–2019. Projections were estimated with linear regression and reported as a 95% prediction interval. Rates outside this interval were considered statistically significant changes. This means that the predictions were based on one-, two- and three-year extrapolations of linear trends for 2020, 2021 and 2022 respectively. To validate, we retrospectively predicted ASMRs for all causes, cancers, dementia, external causes, and cardiovascular and respiratory diseases for 1980–2019 based one-, two- and three-year extrapolations on 10-year linear trends. For 2010–2019 predictions, we calculated mean absolute error per cent (MAE%) and root mean square error per cent (RMSE%), and proportion outside the 95 per cent prediction intervals. The number of deaths in all groups was expected to be more than large enough for normal distribution to be assumed (normal approximation of Poisson distribution). A Durbin-Watson test was used to detect autocorrelation among the annual observations.
Results

In total, 537 757 deaths were reported in 2010–2022, of which 128,218 were reported in 2020–2022. There were 4112 cases of COVID-19 as the underlying cause of death, corresponding to 3.2 percent of all deaths in 2020–2022. Adverse effects of the COVID-19 vaccine were the underlying cause of death in 24 cases, of which 19 were in 2021 and five were in 2022 [sure /sarcasm].
Overall, the cause of death was missing in 9763 cases (1.8%). More details on missing data are found in Supplement 1. In 2020–2022, the cause of death was unknown in 2545 cases (2.0%).
Patient characteristics for deaths are presented in Table 1.
Mortality and excess mortality are presented in Table 2 (number of deaths) and Table 3 (ASMR) for the pandemic years 2020, 2021 and 2022. No significant autocorrelation was observed. There was significant excess all-cause mortality in 2021 and 2022, but in 2020, both the number of deaths and ASMR were within the 95 percent prediction interval. COVID-19 as a share of excess mortality was higher in 2021 than in 2022 both in the number of deaths (58% vs 49%) and as ASMR (72% vs 52%). Apart from COVID-19, excess mortality was most pronounced for cardiovascular diseases in both 2021 and 2022. The number of deaths from cancer was significantly but marginally elevated in 2022, but ASMR was within the 95% prediction interval in all pandemic years. The number of deaths from the “all other causes” group was significantly higher than predicted in all pandemic years, and a significant excess ASMR for this group was observed in 2021 and 2022. There were fewer missing causes of death (N) than predicted in both 2021 and 2022.
Discussion
Key results Excess non-COVID-19 mortality was seen in Norway from October 2021 through 2022 and cumulatively comprised 3632 (46.9%) of 7744 net excess deaths (ASMR 57.3, 40.7%). This was mainly driven by an increase in cardiovascular deaths, accounting for 44.6% of net cumulative excess deaths (ASMR 56.6%). A lack of seasonal increases during winter was observed for dementia and respiratory diseases in 2020 and 2021, which resulted in lower than predicted net cumulative mortality for dementia (N -6.8%; ASMR -13.1%) and respiratory diseases (N -24.4%, ASMR -31.5%). The number of cancer deaths was significantly but marginally higher than predicted in 2022 (3.5% of net excess deaths, ASMR 2.3%). Of the total net cumulative excess mortality, COVID-19 comprised the largest cause (N 51.1%, ASMR 59.3%). The remaining causes, including external causes, comprised 32.2% of net excess deaths (ASMR 32.8%) from March 2020 until December 2022.
Limitations
Central Nordic health registers are generally considered to have a high coverage and contain reliable information…
We cannot rule out that some causes of death were over- or underrepresented in death certificates received [really? /sarcasm] by the register after we extracted data for this study. We do not believe that the biases were sufficient to affect our main findings [so, what about the modRNA jabs?]
The information on COVID-19 status in the register is limited to cases where it was reported as an underlying or contributing cause of death. For example, we did not have any information about previous COVID-19 infection or vaccination status [how wonderful—one cannot enquire about stuff one never bothers to ask about, even though, as per the Institute of Public Health, they know each one’s vaccination status].
The pandemic itself may have influenced how doctors determined causes of death on the death certificate [do tell…] For example, COVID-19 may have changed the level of precision for respiratory causes of death.
One could argue that predictions relying on two- and three-year extrapolations are questionable. Nevertheless, the validation results presented in Supplement 2 suggest that our method provides reliable predictions, even when extending the extrapolation to three years. Mortality displacement is a general challenge when analysing and interpreting excess mortality. From 2010 to 2019, there were no major deviations from mortality trends in Norway that should influence mortality in Norway significantly in the following COVID-19 pandemic years [oddly, cardiovascular disease deaths are literally off the charts…].
In here, a brief remark: the data came from the Institute of Public Health, and, no, the study authors apparently never asked themselves about the vaccination status. Odd, eh? These are quite short ‘results’ and ‘limitations’ sections, hence we move on to the ‘interpretation’.
Interpretation
The excess all-cause mortality in Norway found here is of the same magnitude but slightly higher than previously reported by the Norwegian Institute of Public Health. This is also reflected in the fact that the reduction in life expectancy in Norway in 2022 was the largest since World War II. Excess cardiovascular mortality during the COVID-19 pandemic has been observed in the USA and Mexico. In neighbouring Sweden and Denmark, there was no increase in cardiovascular mortality in 2020–2022. 2020 and 2021 deaths from non-COVID-19 respiratory diseases were lower than predicted in Sweden.
It is possible that a substantial number of registered non-COVID-19 deaths were caused by undetected SARS-CoV-2 infections [we’re back to asymptomatic infections]. There was an increase in excess non-COVID-19 deaths as well as COVID-19 deaths after mid-2021. The increased all-cause mortality coincides with the laxing of anti-infection measures, including lockdown, and with a decrease in routine COVID-19 testing [both isn’t true, for the mandates were lifted in Feb. 2022]. An increase in the number of deaths with unexplained causes in the USA has been observed both during influenza seasons and during the COVID-19 pandemic. Some excess mortality with cardiovascular diseases and cancer, as well as “all other causes” as registered underlying causes of death, could probably be attributed to unintentional ignorance of COVID-19 infection by health personnel [because of asymptomatic infection, right? So, one isn’t hospitalised for Covid, but might have died of/with Covid, is what they are saying here, believe it or not…]. It is also likely that the lifting of restrictions in 2021 led to an abnormally large spread of many respiratory infections in a population particularly susceptible after a long period without exposure to infectious agents [which is why there is lower morbidity from respiratory infections but significantly elevated mortality in the cardiovascular diseases category, right?]
Many people dying from non-COVID-19 causes at the end of the observation period in this study probably had a SARS-CoV-2 infection many months prior to, and apparently unrelated to their death. COVID-19 is a new disease, and thus far, little is known about what long-term effects the infection has on the course of other chronic diseases. The virus may have effects directly on different pathophysiological mechanisms that could lead to increased mortality [‘Long Covid’, PASC, or ‘vaccine injury’, anyone?]. It is also likely that indirect effects on general mortality, such as peri- and postinfectious increased general frailty, malnutrition and wasting or long-COVID syndrome, may have contributed to increased mortality from several causes, including cancer.
There has been concern that lockdowns have resulted in less use of health care, leading to diseases that otherwise would have been discovered remaining undiagnosed, possibly with increased mortality. This may be one explanation for the accelerated reduction in several cardiovascular diseases in 2020 and 2021 according to the Norwegian Cardiovascular Disease Registry [huhum, look, we checked that box]. Routine follow-up consultations for chronic diseases may have been postponed or cancelled due to restrictions, or patients may have been reluctant to attend them due to fear of infection. Diabetes care may have suffered particularly, as increases in diabetes mortality have been observed in both Norway and elsewhere. Studies should be carried out to clarify whether there is an association between the underutilisation of health services and excess mortality from non-COVID-19 causes [sure, let’s pretend there’s no drastic, literally off-the-charts increase in cardiovascular deaths here]. Researchers should also investigate whether the restrictions have resulted in deterioration of lifestyle factors, such as less physical activity, a less healthy diet and even social and mental health issues that influence mortality.
There has been some opposition to mass vaccination during the COVID-19 pandemic due to concerns about potential harmful effects of allegedly insufficiently tested vaccines. There is a temporal concordance between increasing vaccine coverage and increasing excess mortality. From data available to us, it was not possible to compare excess mortality in vaccinated and unvaccinated individuals [even though let’s admit it, the lead author works for the Institute of Public Health, which has that data…so, why not cross-reference it with, say, the cancer or cardiovascular death data? You know, just to be sure…] Preliminary analyses from the National Preparedness Register for COVID-19 in Norway (Beredt C19), do not show any sign of increased mortality among vaccinated older people [22, which is the one reference I’ve kept—for it points to the following study by Lopez-Doriga Ruiz et al., ‘Short-term safety of COVID-19 mRNA vaccines with respect to all-cause mortality in the older population in Norway’, Vaccine 41 (2023): 323-32; note that the lead author also works at the Institute of Public Health; I’ve kept this reference for one reason: ‘We obtained information on dates of vaccination and vaccine product. The two mRNA vaccines Pfizer-BioNTech and Moderna were distributed in Norway from December 27, 2020, and January 14, 2021, respectively…The study exposure was first dose of COVID-19 mRNA vaccine administered between December 27, 2020, and March 31, 2021. The outcome of interest was all-cause mortality during the first three weeks (21 days) after vaccination’. This explains why, exactly, ‘preliminary analyses’ by Raknes et al. didn’t find anything—because the latter’s study ran for another 7 quarters…].
We have previously shown that compared to Sweden, Norway had a lower ASMR for cardiovascular and a higher ASMR for respiratory causes of death in 2010 to 2019. Some of these differences may not be fully explained by differences in morbidity between the countries [which is something someone should also study, I presume]. It is conceivable that there are different traditions in different countries for which causes of death doctors tend to indicate on the death certificate. The introduction of electronic death certificates may have led to Norwegian doctors changing the practice of filling in death certificates to more like how it is done in Sweden.
The lack of seasonal surges in respiratory infections in the winters of 2020/21 and 2021/22 probably contributed to some mortality displacement and thus more deaths than predicted for the rest of the observation period, but it cannot explain all of it.
Death often occurs in very old, multimorbid people, and it can be difficult to reliably determine the underlying cause of death. The lower than predicted dementia mortality may be partly due to fewer deaths from respiratory infections during lockdown.
Generalisability
The generalizability of our findings to other countries should be considered in light of several factors. Although data from the Norwegian Cause of Death Register are known for high data quality and reliability, and thus has excellent internal validity, it is crucial to acknowledge that COVID-19 mortality rates in Norway were relatively lower compared to many similar countries. Furthermore, variations in testing intensity, vaccine coverage, and the stringency of public health measures make comparisons between countries less straightforward. In addition, there are differences in the age composition of the population in Norway compared to other nations. Therefore, while our results provide valuable insights into the Norwegian context, caution should be exercised when applying them to settings with distinct demographic profiles and pandemic response strategies.
Sure, so let’s compare, say, cardiovascular diseases, then? Or add a cross-reference to, say, Covid-19 modRNA vaccination status?
Conclusions
During the pandemic from 2020 to 2022, Norway experienced a significant increase in non-COVID-19 deaths. This rise in mortality, especially notable from late 2021 to December 2022, was primarily seen in cardiovascular diseases. To understand the underlying causes better, further research is essential to determine whether it resulted from the virus itself, the measures taken to control its spread, or other factors.
Sure, grifters of all countries, unite.
Bottom Lines
There’s so much that could be said (and that, in fact, I’ve mentioned in these pages; just look for ‘covid’ and ‘Norway’ using the search function).
This is an amazingly blind study. Scandinavian countries have very high levels of data integrity, yet it’s exceptionally strange to see study after study after study that avoids cross-relational analysis of the one thing that might shed (no pun intended) some light on the off-the-charts cardiovascular-associated ‘significant excess’ mortality.
I suppose that we’ll learn more about cancer rates around April when the next cancer report is due.
Until then—I shall ask the corresponding author about the two main issues, and should I hear from them, I’ll let you know.
In the meantime, save a thought and/or prayer for those who suffered and died.





Not strange at all, really. You ask for funding for a specific study, well-defined in scope and scale, and expanding the scope after having been granted funding is not what you are supposed to do; you may even be prosecuted for misappropriation of funds, which is correct procedure.
Where to look is who is granting funding for research-proposals. That information, if not disclosed in the study, should be public and available on request from the researchers.
But asking the researchers why they didn't include vaccination-status, or asking the board granting funding if they would have done so had vaccination-status been included would not be well-received. Expect stonewalling and possible problems at work, via backchannel-messaging: you do live in the nation of Jante-loven after all, so being right/correct matters much less than does being (thinking/feeling) the same as all others.