Covid in Norway: A Pandemic for All Seasons
'News' from Up North About Sars-Cov-2: Legacy Media 'Reporting' Offers 'New' Spin While a New Study Indicates Elevated Risks for Mothers if 'Infected Multiple Times'
It almost feels like Groundhog Day all over again, albeit with a deadly serious twist: unlike that funny movie from a very much bygone era, the WHO-declared, so-called ‘Corona Pandemic™’ has largely vanished from legacy media.
That is, until it pops up every now and then, as evidenced by last month’s—very much unexpected state broadcaster NRK’s discussion of modRNA injectable-induced adverse events:
Today, I have two items from up north for you, dear readers: first, a brief legacy media piece and, secondly, ‘news’ from the Norwegian Institute of Public Health (IPH), which published the results of a new study about repeat infections and risks for pregnant women and their children.
As always, translations and emphases mine.
The Experts Answer About ‘Long Covid’
By Jan-Erik Wilthil, NRK, 1/2 Nov. 2023 [source]
How dangerous is the coronavirus now? Is there a high chance of long-term effects? Should I take the updated vaccine? Now you can get answers to all your questions about ‘long covid’.
Almost four years after it was first discovered in Wuhan, China, the coronavirus still poses a serious health threat.
Although the virus is no longer as deadly, many people are still on long-term sick leave due to exhaustion after being infected.
[this is awful, for, according to official data from the social insurance provider NAV, there ‘never have been more people on sick-leave than in Q2 of 2023’; as the dedicated ‘study’ explains, ‘a strong association between covid-19 sickness absence and “weakness/tiredness general”-sickness absence was found’, which, to the researchers’ surprise (sic), affects 30-34 year-old disproportionately]
Researchers around the world are working to find out why people are affected by ‘long covid’. New serious after-effects of the virus are constantly being uncovered.
Just this week, a Nordic study showed that the risk of stillbirth increases for pregnant women who have fallen ill with COVID-19 earlier [this is the second item I discuss at length below].
At the same time, health authorities fear that half of Norway's population will be infected this winter [odd, for about 80% of residents, according to official data, received at least two jabs…].
Some studies also indicate that the risk of late effects increases if you are infected several times. Nevertheless, the NIPH will not recommend the updated vaccine for those under the age of 65.
In other words, the pandemic is far from over, and many questions remain unanswered.
NRK has therefore assembled a panel of experts who can answer your questions about the coronavirus and ‘long covid’.
There is already a great deal of interest. The experts are answering as many questions as they can, and you may get your answers by reading the questions that are being answered.
This is the expert panel
The experts have different backgrounds and do not necessarily agree on everything.
[Experts™ incl. Espen Rostrup Nakstad, MD, deputy director of health and human services and known BS-spreader; Arne Søraas, researcher in infectious diseases at the U of Oslo; and Anne Spurkland, professor of immunology at the U of Oslo]
I’ll spare you most of the currently (Thursday morning local time) ongoing Q&A, but I shall reproduce the first question and answer to indicate the one and only, albeit super-dooper major flaw in Norway’s current ‘discussion’ of the issue:

Jostein Lynum (12 hours ago)
Hello. Do unvaccinated or vaccinated people get long covid? Why is it possibly so?
I am not a vaccine supporter and have survived this pandemic. Can someone on the expert panel explain why?
I expect good and comprehensive answers.
No BS here, it’s the one and only (in my opinion) valid question here.
Arne Søraas *Expert [lol] (26 minutes ago)
We have published results on this in the Corona study.
The vaccine protects against long-covid, but not as much as I personally would have thought/hoped.
https://pubmed.ncbi.nlm.nih.gov/36375693/
Even for the unvaccinated, covid is usually not dangerous, so that is probably why you have survived if you have had the disease [I don’t know if this is meant to be ironic]. If you haven't had the disease and are unvaccinated, you know what I'm going to say: run and get vaccinated! [the ‘updated’, monovalent BioNTech/Pfizer XBB.1.5 jabs are offered throughout Norway, which, according to official data published by the IPH, is on its way out; currently, it’s the EG.5.1.X and BA.2.86 variants that dominate, which, of course, begs the question as to why anyone who’s ‘unvaxxed’ should get the XBB.1.5 jabs now…]
I myself have wondered whether the vaccine (which, after all, contains/stores a protein from the virus itself [false, it contains modRNA that makes human cells manufacture a synthetic version of such a protein, not ‘a protein from the virus itself’]) can cause long-covid. I have looked at this myself in data from the Corona study, but it has not been published. I saw no such effect. So: I didn’t see any ‘long vaccine’ in our data, and that’s good. At the same time, there are other known side effects from the vaccine, of course.
While we’re on the topic, I shall refrain from posting more of these Q&As right now (personally, one of these BS Bingo ‘answers’ is more than enough, but there are more than a hundred questions outstanding, we’ll have to see if we get some more later on).
Let’s do something else by way of moving on, shall we?
What Does the IPH Recommend these Days to Fight Covid?
According to the current guidelines, there is literally nothing new: there’s no contraindication for, say, ‘unvaccinated but recovered’ individuals (which is different from literally all other injectable products); pregnant women and anyone else can and should take as many jabs of the current modRNA sauce and/or other shots (here’s looking at you, influenza vaccines).
The most odious notion here is, of course, the following recommendation:
mRNA vaccines against COVID-19 can be used during pregnancy and breastfeeding.
And this is the topic we’ll address now as we take a closer look at the above-mentioned new Nordic study about the Covid modRNA injections Corona infection, pregnancy, and births.
Magnus et al., ‘Infection with SARS-CoV-2 during pregnancy and risk of stillbirth: a Scandinavian registry study’
BMJ Public Health 2023;1:e000314. doi: 10.1136/bmjph-2023-000314 [direct link]
All emphases and commentary mine; for readability, I’ve omitted all references (which are available in full by clicking on the above link).
Abstract
Background A few studies indicate that women [no woke-ism here] infected with SARS-CoV-2 during pregnancy might have an increased risk of stillbirth. Our aim was to investigate the risk of stillbirth according to infection with SARS-CoV-2 during pregnancy also taking the variant into account.
Methods We conducted a register-based study using the Swedish, Danish and Norwegian birth registries. A total of 389 949 births (1013 stillbirths) after 22 completed gestational weeks between 1 May 2020 and end of follow-up (27 January 2022 for Sweden and Norway; 31 December 2021 for Denmark). We estimated the risk of stillbirth following SARS-CoV-2 infection after 22 completed gestational weeks using Cox regression for each country, and combined the results using a random-effects meta-analysis.
Results SARS-CoV-2 infection after 22 completed gestational weeks was associated with an increased risk of stillbirth (adjusted HR 2.40; 95% CI 1.22 to 4.71). The risk was highest during the first weeks following infection, with an adjusted HR of 5.48 (95% CI 3.11 to 9.63) during the first 2 weeks, 4.38 (95% CI 2.41 to 7.98) during the first 4 weeks, and 3.71 (95% CI 1.81 to 7.59) during the first 6 weeks. Furthermore, the risk was greatest among women infected during the Delta-dominated period (adjusted HR 8.23; 95% CI 3.65 to 18.59), and more modest among women infected during the Index (adjusted HR 3.66; 95% CI 1.89 to 7.06) and Alpha (adjusted HR 2.73; 95% CI 1.13 to 6.59) dominated periods.
Conclusions We found an increased risk of stillbirth among women who were infected with SARS-CoV-2 after 22 gestational weeks, with the greatest risk during the Delta-dominated period.
So, at first sight, a well-populated study, right? Let’s dive into the paper and look for more clues, shall we? Do note, however, the absence of any indication that says ‘vaccination status’, which I think is the main methodological problem here.
We studied live and stillbirths after 22 completed gestational weeks in Sweden, Denmark and Norway between 1 March 2020 and end of follow-up (27 January 2022 for Sweden and Norway; 31 December 2021 for Denmark). Births were identified through the Swedish Pregnancy Register, the Danish National Patient Register (registrations of International Classification of Disease version 10 codes Z38, O80–84 and P95), and the Medical Birth Registry of Norway. The small number of late induced abortions conducted after 22 completed gestational weeks were excluded (n=110 for Denmark; n=23 for Norway; information not available for Sweden). The Danish and Norwegian data included all births nationally, while the Swedish data included 94% of all births in Sweden (in 18 of 21 Swedish regions).
Sounds ok-ish to me so far, but as soon as we read on, there arise further methodological concerns
We only included singletons and only the first registered birth to each woman during the study period. To avoid oversampling of preterm pregnancies towards end of the study period, we excluded pregnancies without the possibility to reach 42 completed weeks by the end of follow-up. We obtained information on maternal socioeconomic measures, infections with SARS-CoV-2, and vaccination against SARS-CoV-2 from national databases using unique national identification numbers.
Oh, look, no preterm problems were included, which is a major red flag (see below).
Moreover, the study authors ‘obtained information on…vaccination’, too. Shall we guess whether or not this piece made it into the study?
Sars-Cov-2 Infection
The exposure of interest was a positive test for SARS-CoV-2 after 22 completed gestational weeks up until the day before delivery. Our hypothesis is that infection may increase the risk of fetal death. Thus, infection before gestational week 22 might increase the risk of fetal death prior to 22 completed weeks (miscarriage), which could affect our results when only looking at fetal deaths after 22 gestational weeks (stillbirths).
See what I meant about the exclusion of preterm pregnancies? They were excluded from the get-go, hence there’s a gaping hole in the set-up.
We did not exclude women with infection prior to 22 gestational weeks from the analysis, but adjusted for this as a covariate. In addition, we conducted a sensitivity analysis excluding pregnancies to women infected during pregnancy prior to 22 completed gestational weeks.
Nice, but how could doing so ‘compensate’ in any way, shape, or form for the absence of analytical consideration of the pregnant women’s ‘vaccination status’?
Covariates
We obtained information on maternal age at the beginning of pregnancy (continuous), parity (0, 1, 2 or more), educational level (9 years or less, 10–12 years, more than 12 years), household income in tertiles based on the national distribution (first, second and third tertile), living with a partner (yes or no), region of birth (Scandinavia, Other European countries, Middle East/Africa, other/unknown), smoking in pregnancy (yes or no), pre or early-pregnancy body mass index (continuous), pre-existing chronic condition (yes or no) prior to pregnancy and vaccination against SARS-CoV-2 (none, before pregnancy, during pregnancy). A general recommendation for vaccination of all pregnant women was issued in May 2021, in Sweden, August 2021, in Norway and July 2021, in Denmark. Pre-existing chronic conditions prior to pregnancy included hypertension, chronic kidney disease, asthma, cardiovascular disease, thrombosis and diabetes.
Statistical Analysis
In multivariable analyses, we adjusted for age, parity, educational level, household income, living with a partner, region of birth and a time-varying variable of vaccination against SARS-CoV-2. We also adjusted for infection with SARS-CoV-2 during pregnancy prior to 22 completed gestational weeks in the main model…
In secondary analyses, we evaluated differences in the risk of stillbirth according to a positive test during time periods dominated by different variants of SARS-CoV-2; (Index (prior to 1 February 2021), Alpha (between 1 February 2021 and 30 June 2021) or Delta (between 1 July 2021 and 31 December 2021)).
Results
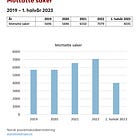
Across the three countries, there were 389 949 births during the study period (figure 1), with 184 771 in Sweden, 106 991 in Denmark and 98 187 in Norway. Among these births, 1013 (3 per 1000) ended in a stillbirth (3 per 1000 in Sweden, 3 per 1000 in Denmark and 2 per 1000 in Norway). There were 8855 births (2.3%) to women with a positive test for SARS-CoV-2 in pregnancy after gestational week 22 (3.2% in Sweden, 1.7% in Denmark and 0.9% in Norway). Among women with positive tests after 22 gestational weeks, a total of 31 women had a subsequent stillbirth. Women who tested positive for SARS-CoV-2 during pregnancy had a slightly higher parity, lower educational level, lower income, were more likely to be from the middle East/Africa, and had a slightly higher prepregnancy body mass index, compared with women who did not test positive during pregnancy…
All of the 31 exposed cases of stillbirth occurred among unvaccinated women. These exposed cases were infected between 31 March 2020 and 28 October 2021. Most exposed stillbirths (19 of 31) occurred within 3 weeks after a positive test. We observed an increased risk of stillbirth among women who were infected with SARS-CoV-2 after 22 completed gestational weeks, with an incidence rate of 6 per 100 000 exposed follow-up days and 2 per 100 000 unexposed follow-up days, with a corresponding adjusted HR of 2.40 (95% CI 1.22 to 4.71), and evidence of heterogeneity between countries (I2 68%; p=0.04; table 2). We also found that only four of the exposed cases of stillbirth were to women who had been admitted to the ICU during pregnancy for COVID-19. The risk of stillbirth was highest during the first weeks after infection with SARS-CoV-2, with an adjusted HR of 5.48 (95% CI 3.11 to 9.63) during the 2 weeks following infection, 4.38 (95% CI 2.41 to 7.98) during the 4 weeks following infection, and 3.71 (95% CI 1.81 to 7.59) during the 6 weeks following infection (table 2).
I read this the following way: there were 31 stillbirths that occurred exclusively among ‘unvaccinated’ women, and despite the granularity of data in Nordic statistics, they never clearly state which of the indicators mentioned—’lower educational level, lower income, were more likely to be from the middle East/Africa, and had a slightly higher prepregnancy body mass index, compared with women who did not test positive during pregnancy’—were associated with these 31 women.
We know that ‘vaccine hesitancy’ was (is) higher among individuals who fall into any of these categories, and since all people in the study population are clearly identifiable, this would have to be easily do-able (but for whatever reason wasn’t done).
Strangely, the section on limitations adds yet another issue:
We did not have any information on causes and classifications of stillbirths in the birth registries, including clinical information from autopsies or placental histopathological analysis. Furthermore, no information on SARS-CoV-2 infection of the fetus was available. We were also unable to look at the risk of stillbirth according to the gestational week of infection with SARS-CoV-2 in more detail due to the small number of exposed cases…
We were unable to distinguish the risk of stillbirths prior to the onset of labour and stillbirths arising intrapartum according to infection with SARS-CoV-2 due to small numbers. We also did not have any information on treatment for SARS-CoV-2, and we could, therefore, not evaluate how it might have impacted the subsequent risk of stillbirth. Finally, we had limited ability to evaluate the proportional hazards assumption due to the small number of exposed cases of stillbirth.
All told, this is not a very helpful study but an exercise in futility. In their conclusion, the authors throw away their integrity:
In this Scandinavian registry-based study, infection with SARS-CoV-2 was associated with an increased risk of stillbirth, with the greatest risk among women exposed to the Delta variant, although the small number of exposed cases yielded uncertain estimates for the individual variants. We also did not have information available on the fetus’ infection status. However, our findings highlight the need for further understanding of differences in risk of pregnancy complications according to SARS-CoV-2 variants. The tendency for an increased risk of stillbirth among women infected with SARS-CoV-2 during pregnancy highlights the importance of vaccination of pregnant women which was recommended across most countries.
Two things to note: first, note all the ‘we’re unable to determine’ items listed in the limitations vs. the bold statement that ‘infection with SARS-CoV-2 was associated with an increased risk of stillbirth, with the greatest risk among women exposed to the Delta variant’.
Second, the ‘importance of vaccination’ was not really substantiated to me, as the blanket statement that all 31 cases of stillbirths occurred among ‘unvaccinated’ were not followed-up by, say, investigation about possible contraindications of these modRNA products.
Moreover, since the Delta variant no longer exists, it’s kind of a moot point to figure this out, eh?
How Does the IPH Spin this?
Well, read for yourself (source):
Women who were infected with COVID-19 during pregnancy had an increased risk of stillbirth. This is according to a large new Nordic study. The risk was greatest among those who had the infection during the period when the delta variant of the virus was circulating.
The aim of the study was to investigate whether the risk of stillbirth after 22 completed weeks of pregnancy was higher among women who had tested positive for COVID-19 during pregnancy. Stillbirth is very rare, making it difficult to detect any increased incidence. The study therefore combined data from national health registries in Norway, Sweden and Denmark to obtain large enough numbers to analyse. The study included 389,949 births across the three countries, with a total of 1,013 stillbirths, of which 31 were among women who had had a COVID-19 infection. This represented a 2.4 times higher risk of stillbirth among women who had had COVID-19 during pregnancy.
‘Previous studies that have tried to look at this association have had very small numbers and have therefore not been able to come up with robust conclusions’, says Maria C. Magnus, senior researcher at the Centre for Fertility and Health.
‘We would also like to point out that stillbirth is very rare’, says Magnus, emphasising that this also applies to those with a corona infection during pregnancy.
The absolute risk of stillbirth was 2.3 per 100,000 follow-up days among pregnant women who had not had COVID-19 during pregnancy, while it was 5.8 per 100,000 follow-up days among those who had tested positive for COVID-19 while pregnant. In total, there were only 31 stillbirths among those with a positive COVID-19 test during the study period…
Risk greatest shortly after infection
The study examined the risk of stillbirth in different time periods after infection with COVID-19.
- "We found that the risk was highest in the first two weeks after infection, with a 5.5 times higher risk in the first two weeks," says Magnus.
The risk was lower, but still elevated, the longer it had been since the woman was infected, with a 4.4-fold increased risk in the first four weeks after infection, and a 3.7-fold higher risk in the first six weeks after infection.
‘The fact that the risk was highest shortly after infection supports the possibility of a causal relationship’, says Magnus.
‘One limitation of the study is that we used the date when the woman was registered with a positive test for COVID-19 in national surveillance registers to calculate when she had the infection. This results in some misclassification with regard to the time window, as it probably varies how long the women waited to take a test when they were sick,’ Magnus adds. [surely, this is the main thing to mention here, eh?]
The significance of the findings for vaccination
The Norwegian Institute of Public Health recommends that all pregnant women should have a booster dose of coronavirus vaccine in the second or third trimester of pregnancy. The recommendation is based on an overall assessment of findings from various studies that show an increased risk of serious illness and pregnancy complications among pregnant women who have had an infection with COVID-19, and that there is no risk to the mother, child or the course of pregnancy from taking the vaccine.
Well, let’s see how long that news item stands before it is amended, right?




These women who lost their children during delta were all freshly vaccinated. That's what the data suggest.
https://substack.com/@covdata/note/c-42934035?utm_source=notes-share-action&r=qtkkb
https://vigilance.pervaers.com/p/us-summer-deaths-of-2021
They're pushing masks again in Australia saying it's the 'eighth wave.'
It's 37C.
Shouldn't we be in the climate narrative? It's all so tiresome.